Scientists show high levels of hostility aggression, and conscientiousness compared to the general population, at least according to psychologists. As a scientist and a manager of scientists, I agree but would add another trait: fear of failure.
Science is supposedly distinguished from other forms of knowledge by falsifiability: if a statement cannot be disproven it belongs to the realm of faith rather than that of science. Much of the phage therapy literature is little better than shamanism: we gave the treatment, the patients got better, therefore PT works. Given that placebos cure infectious diseases at rates of 35-80%, such observations are useless and misleading.
The advancement of phage therapy is hindered immensely by the prevalence of true-believerism among its practitioners. The result is a paucity of well-controlled trials and an oversupply of observational studies. These are notoriously subject to selection bias, in which only the apparent successes get published (and then lead to book deals). This is no way at all to move a technology forward.
Learning to fail, and fail quickly, is the quickest route to success. There are many more ways in which a treatment can fail than ways in which it can succeed. Identifying failure modes allows you to identify dead ends and eliminate them from your product development path.
That’s why this paper, which examines the robustness of a phage enzyme treatment of infection, is so encouraging. It examines several failure modes for different phage capsular depolymerases in a mouse model of E coli infection. Encapsulation allows bacteria to better evade the immune system and is a virulence factor that promotes the establishment of infections.
Capsules also block phage infection of bacteria, and so under the principle that phage always evolve a response to every host defense, some phage encode enzymes that break down capsules. In principle that should render the bacteria more susceptible to clearance by the immune system, and indeed there is some evidence of this (see here and here).
To their great credit, Lin et al at the University of Texas asked whether the timing and route of depolymerase administration would cause it to fail, and whether there was a difference between purified enzyme vs whole phage.
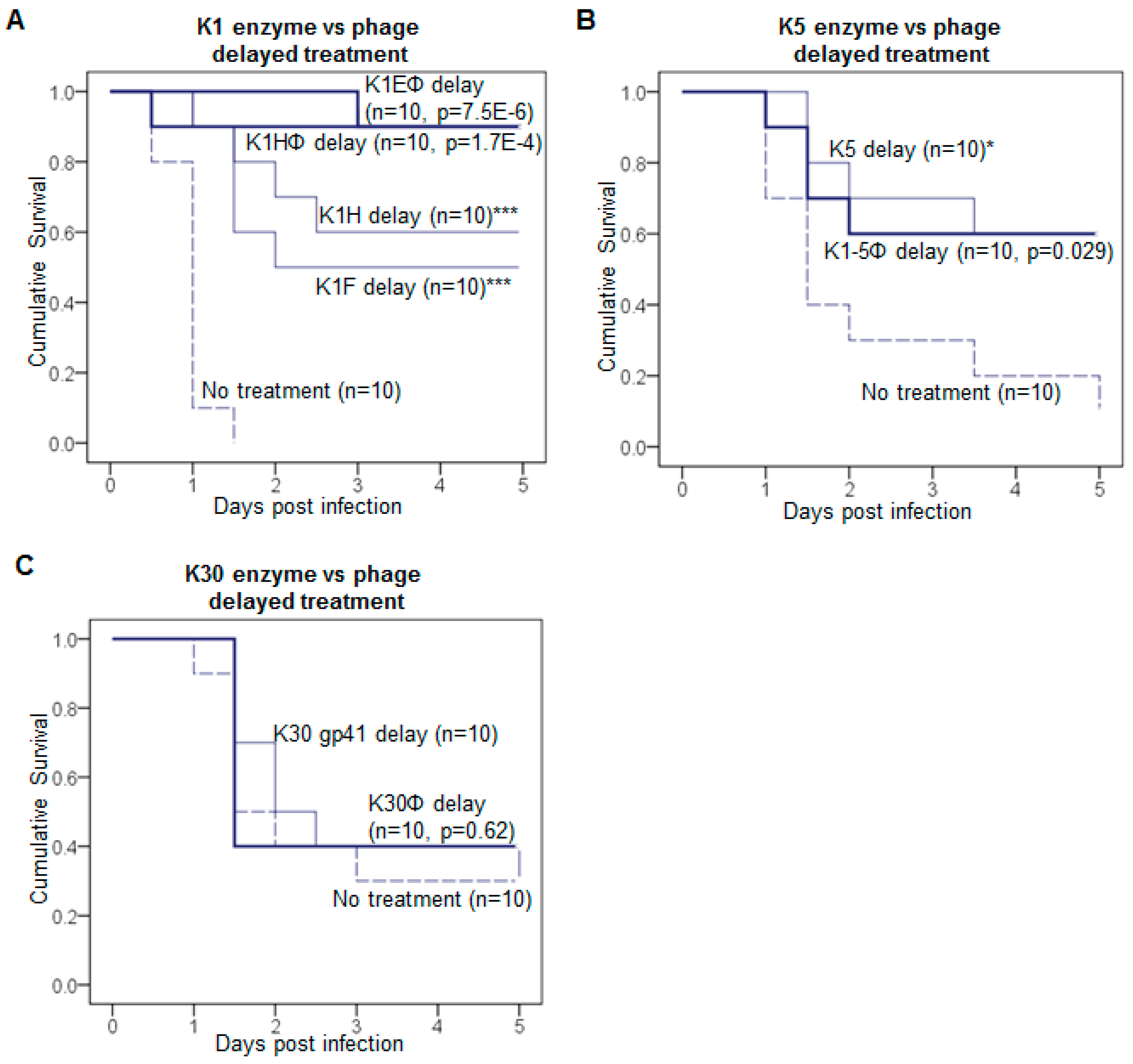
The answer, as always in biology, is “it depends”. Some enzymes did better than others after a delay. Some phages did better than purified enzymes, others did worse:
From Antibiotic Therapy Using Phage Depolymerases: Robustness Across a Range of Conditions
It’s confusing, but that’s OK. We are a long way from seeing these enzymes in the clinic, if ever. As biologicals, they will be much more expensive than antibiotics and will require injection rather than oral administration. Each enzyme is specific not only to a single bacterial species, but to a particular strain within that species. But those issues can be solved, at least for some applications and indications.
The real import of this paper, at least for me, was seeing academic PT scientists express some long-overdue skepticism toward their own projects:
Offsetting the now many laboratory studies of phages and phage products showing positive results, the few clinical phage therapy trials conducted under standards of Western medicine have actually failed….The contrasting outcomes between actual trials and laboratory infections raise the possibility that experimental studies poorly represent applications.
Yes, they do indeed raise this possibility. The sooner phage scientists start accounting for it, the sooner we might actually see PT become a reality. And learning how and why PT fails is the only way to get there.