The time required to recover from antibiotics is somewhere between zero and infinity.
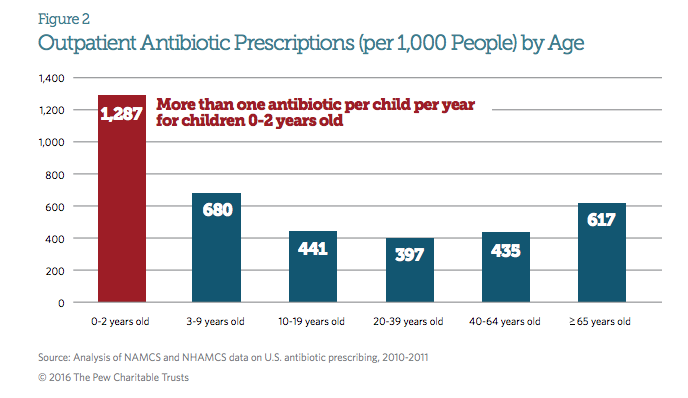
Antibiotics target bacterial proteins and (for the most part) have no direct effect on human proteins, cells or tissues. Antibiotics in general, and ß-lactams and cephalosporins in particular, are so free of acute adverse effects (the “zero” scenario) that physicians often hand them out like candy [1] [2] .
But antibiotics might be worse for you than candy [3] . Antibiotics don’t distinguish between “good” and “bad” bacteria. Not surprisingly, they can disrupt your gut microbiome [4], resulting in transient diarrhea.
Usually these effects are short-lived, especially in adults. If that was always the case, then we could say that antibiotic effects persist for no more than a week or two.
But it’s not. Changes in microbiome composition after clindamycin treatment have been found to persist for more than two years [5]. Long-term therapy – such as for tuberculosis – results in far more profound and disruptive change, long after cessation of therapy [6]. And low-level long-term exposure – which is likely if you live downstream from a livestock-feeding operation – also produces changes in gut microbiota [7] .
Infant microbiomes, which are not nearly so well established, are far more susceptible to disruption by antibiotic treatment [8] . Unfortunately, infants are also the most likely to truly need antibiotics, as their immune systems are not well-developed.
Antibiotic exposure, particularly in early life, has been linked to obesity [9] , Type 1 [10] and Type 2 [11] diabetes, arthritis [12] , depression [13], and asthma [14]. We don’t have cures for any of these diseases. So if these associations do indeed pan out as being antibiotic-caused, it would be fair to say that we never recover from antibiotic use: the time required for our bodies to recover is infinity.
Footnotes
[1] http://www.pewtrusts.org/~/media…
[2] Antibiotic prescribing for adults in ambulatory care in the USA, 2007-09.
[3] Relationship between Added Sugars Consumption and Chronic Disease Risk Factors: Current Understanding.
[4] Antibiotics and the gut microbiota.
[5] Long-term ecological impacts of antibiotic administration on the human intestinal microbiota.
[6] Antibiotic treatment for Tuberculosis induces a profound dysbiosis of the microbiome that persists long after therapy is completed.
[7] Obesity in the United States – Dysbiosis from Exposure to Low-Dose Antibiotics?
[8] Infant antibiotic exposures and early-life body mass.
[9] Antibiotic Exposure in Early Life Increases Risk of Childhood Obesity: A Systematic Review and Meta-Analysis.
[10] The effect of past antibiotic exposure on diabetes risk.
[11] Use of Antibiotics and Risk of Type 2 Diabetes: A Population-Based Case-Control Study.
[12] Gut microbiota-host interactions and juvenile idiopathic arthritis
[13] Antibiotic exposure and the risk for depression, anxiety, or psychosis: a nested case-control study.
[14] Low gut microbiota diversity in early infancy precedes asthma at school age.
