The evidence for a link between gut bacteria and depression/anxiety disorders is compelling.
The gut microbiome of clinically depressed patients is substantially altered [1], and gut disorders such as Inflammatory Bowel Disease show both an altered microbiome and an increased risk of depression [2] . We also know that recurrent antibiotic use, which inevitably disrupts the gut microbiota[3] , is associated with an increased risk of depression [4].
But these are just correlations. People who have IBD or are taking antibiotics feel terrible and it’s not surprising that they might be at risk of depression. And even if there are no comorbidities associated with depression, the arrow of causality could run from depression to the microbiome, not the other way around. Depressives might alter their eating habits and engage in other behaviors that affect the microbiome.
More compelling evidence comes from studies with germ-free mice and rats. These animals, which lack a gut microbiome altogether, show altered levels of anxiety [5] , which can be reversed by ingestion of Bifidobacteria or by fecal transplantation from normal mice [6] . Different mouse strains show different basal levels of anxiety. Transplantation of fecal microbiomes between them, or to germ-free mice, results in stress-related behavior similar to that of the donor [7].
Interventions that alter the microbiome affect depressive behavior in both rodents and humans. Probiotics reduce anxiety in rats and alleviate psychological distress in humans [8] . Galacto-oligosaccharides, a prebiotic known to modulate microbiome composition, reduce anxiety and the levels of the stress hormone cortisol in human volunteers [9] . The anxiety-relieving effects of probiotics are blocked in mice when their vagus nerve (which runs between the gut and brain) is cut [10] . This is powerful evidence of a direct link between the gut microbiome and the brain.
We know that gut microbiota synthesize neurotransmitters and their precursors, and that microbiome composition can alter the levels of these transmitters in the central nervous system [11] .
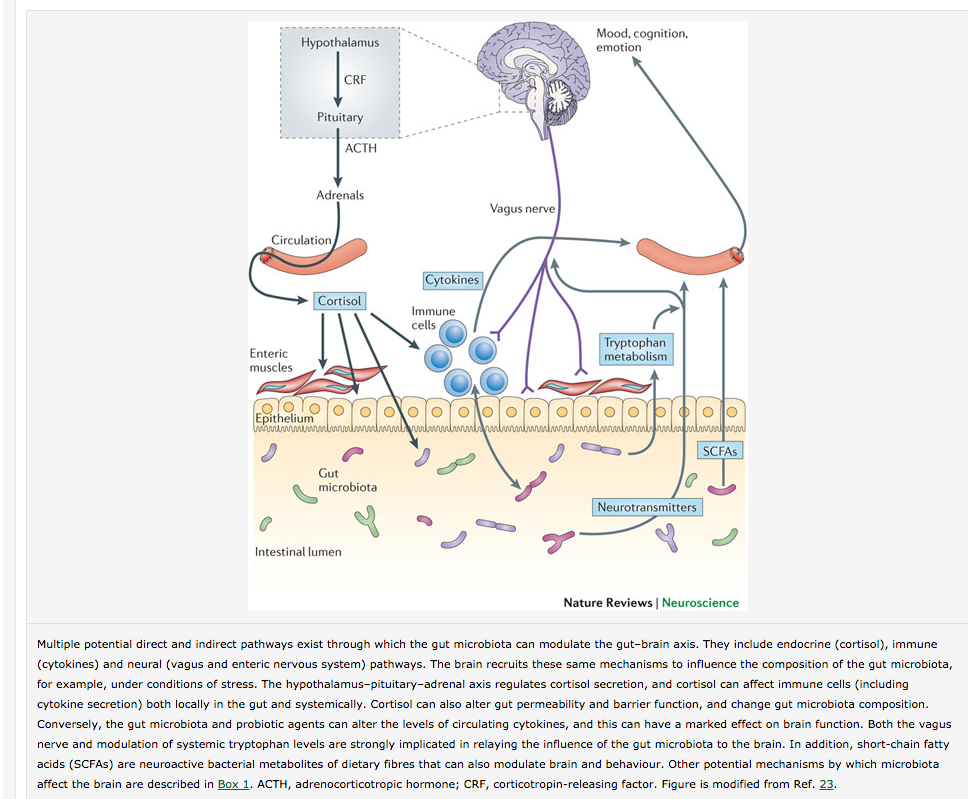
The mechanisms by which the microbiome influences mood and depression are complex and are still being worked out and probably include the immune system. Much of what we know is summarized in this figure:
From Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour.
Links between gut microbiota and mental health have been suggested since the earliest days of microbiology [12] . We now have the tools to investigate these links, and use them to improve mental health and relieve suffering. This is a big deal.
Footnotes
[1] Correlation between the human fecal microbiota and depression.
[2] Anxiety and depression comorbidities in irritable bowel syndrome (IBS): a systematic review and meta-analysis.
[3] Antibiotic use and microbiome function.
[4] Antibiotic exposure and the risk for depression, anxiety, or psychosis: a nested case-control study.
[5] Absence of the gut microbiota enhances anxiety-like behavior and neuroendocrine response to acute stress in rats.
[6] Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice.
[7] The intestinal microbiota affect central levels of brain-derived neurotropic factor and behavior in mice.
[8] Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and… – PubMed – NCBI
[9] Absence of the gut microbiota enhances anxiety-like behavior and neuroendocrine response to acute stress in rats.
[10] Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve
[11] Serotonin, tryptophan metabolism and the brain-gut-microbiome axis.
[12] Intestinal microbiota, probiotics and mental health: from Metchnikoff to modern advances: Part I – autointoxication revisited.

That’s interesting that people with irritable bowel syndrome would be more likely to have depression. I wonder if that is because they have bad bacteria in their system. I feel like it would be useful to get some help from a gastroenterologist to see if that could help your depression.