Phage therapy has been wandering through the wilderness for many decades. It was intensively studied in the 1920’s but fell out of favor in the 1930’s due to inconsistent results and adverse effects. The introduction of sulfa drugs, and then penicillin, rendered it obsolete.
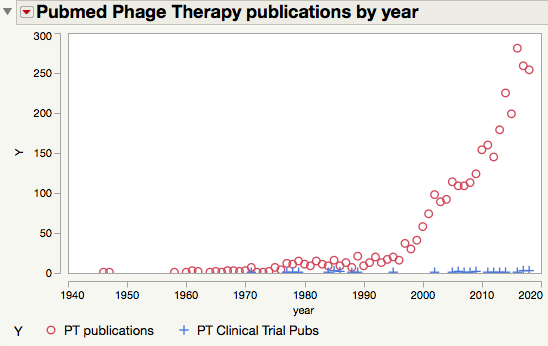
But only for a while. Antibiotics were not the end of history for infectious disease. Resistance emerged in the 1940s, and clinical concerns became significant in the 1960s. Editorials suggesting that phage therapy could be a solution to resistant infections began appearing in the 1960s. They’ve been a staple of science journalism ever since, with “fresh takes” that sound very much like old takes being published in the 1980s , 1990s , 2000 , 2001, 2002 , 2003, 2004, 2005, 2006, 2007 , 2008, 2009 , 2010, 2011, 2012, 2013, 2014, 2015, 2016, 2017, and of course 2018.
You may have noticed that the antibiotic resistance crisis has not been solved by phage therapy. Nor is this likely. But that doesn’t mean that phage therapy is a scam or even that it is doomed to failure. The principle of phage therapy is sound. Its development has been hindered by unfavorable economics and poor execution. I’ve written about these issues a number of times; you can read my takes (fresh and otherwise) here.
However, I do think we may be at a turning point. The risk-reward ratio of developing antimicrobial agents, including conventional antibiotics, remains terrible. Big Pharma is not going to develop PT. But the resistance crisis is starting to attract attention and real money from governments and NGOs. A hundred million dollars would go far in taking PT through the valley of death that lies between where it is now (one-offs run by academics and clinicians with no experience in product development) to where it needs to be (rigorous preclinical formulation and testing along with full QA/QC/GMP implementation).
Antibiotics are the most effective medicines ever discovered. It’s unrealistic to imagine that PT will substantially replace them. Phage have poor pharmacokinetic and biodistribution properties, as well as a tendency to provoke an immune response, that make them unsuited for treating systemic infections.
But they also have several advantages over antibiotics as well. Phage are intrinsically narrow-spectrum, targeting only one bacterial species and sparing the rest. Antibiotics tend to carpet-bomb pathogens and commensals alike, disrupting the microbiome, leading to increased risk of other diseases. Phage therapy may lessen these risks. Phage also encode enzymes that disrupt the biofilms that form in many chronic infections and render them insensitive to antibiotics [23] [24] .
Here are a few promising applications for phage therapy:
- Diabetic foot and leg ulcers. These infections are often unresponsive to antibiotics and lead to amputation at shockingly high rates. Phage – perhaps in combination with normal skin commensals like S. epidermidis, Corynebacter and Propionibacterium species – could eliminate bad bugs like S. aureus and promote healing.
- Pseudomonas infections are common in cystic fibrosis patients and are a major source of suffering and death. Antibiotic therapy is not very effective – these bugs become resistant quickly and also form protective biofilms. A well-formulated phage cocktail could break down biofilms and attack and possibly eradicate these infections.
- Bacterial vaginosis is widespread and increases the risk of contracting STDs and of complications during pregnancy. Phage therapy, targeting specific problem bugs such as Group B Strep could restore a healthy vaginal microbiome, particularly during pregnancy when antibiotics may be contraindicated [25] .
Phage therapy is far from being ready for prime-time. And it is never going to “solve” the antibiotic resistance crisis. But there is absolutely no reason why it cannot be employed to address significant clinical problems and reduce human suffering. All it will take is money and a lot of hard work from smart people.
Footnotes
[1] Staphylococcus phage lysates: an immuno-biological therapy for the prevention and control of staphylococcal disease.
[2] https://www.ncbi.nlm.nih.gov/pmc…
[3] The Good Virus | DiscoverMagazine.com
[7] Set a Microbe to Kill a Microbe
[8] New dawn for phage therapy.
[9] Bacteriophage therapy: a revitalized therapy against bacterial infectious diseases.
[10] Phage Therapy – Everything Old is New Again.
[11] Bacteriophages: an appraisal of their role in the treatment of bacterial infections.
[12] Bacteriophages: Beyond Antibiotics
[13] Bacteriophage Therapy: Exploiting Smaller Fleas | Clinical Infectious Diseases | Oxford Academic
[14] Bacteriophages as potential new therapeutics to replace or supplement antibiotics.
[15] Bacteriophages as a New Drug
[16] Are Phage Viruses the Forgotten Cure for Superbugs? [Excerpt]
[17] Phages may be key in bacteria battle
[18] Phage Therapy Gets Revitalized
[19] Revisiting phage therapy: new applications for old resources
[20] Soviet-era treatment could be the new weapon in the war against antibiotic resistance
[21] Resistant Superbugs Meet Natural Foe in Phage Therapy | GEN
[22] Bacteriophage: A solution to our antibiotics problem? How we can us a virus to fight bacterial infection
[23] Activity of Bacteriophages in Removing Biofilms of Pseudomonas aeruginosa Isolates from Chronic Rhinosinusitis Patients.
[24] Bacteriophage therapy for Staphylococcus aureus biofilm-infected wounds: a new approach to chronic wound care.
[25] Applications for Bacteriophage Therapy during Pregnancy and the Perinatal Period

Hi Drew,
Thanks for the nice post. I was wondering where to find the articles or documents for the “adverse effects” of phage therapy you mentioned?
Thanks,
Aycan
Hi Aycan – Adverse events are fairly rare in modern phage studies. They were much more common in the early days (1920s-1930s). I suspect contamination with endotoxin (which no one knew about then) was the main culprit. But I don’t have a good summary ready at hand – I may have to round one up in a future post.
It’s important however to have all of the facts. Starting with the building a better gut, the good bacteria, the important probiotics and prebiotics along with diet. There is also more info about phage therapy, things people need to first consider and understand.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC90351/
This comment isn’t spam, so I’m posting it. But it is utterly inane. There is no solid evidence as to how to build a better gut etc. and the linked reference is from 2001, hardly a good source of current info on PT.