As with any other viral infection, the principal methods are direct detection of the virus or detection of antibodies generated in response to viral infection.
Direct detection is done by detecting viral proteins or nucleic acids (DNA or RNA). Because nucleic acids can be amplified by PCR and similar technologies, these tests are usually the most sensitive.
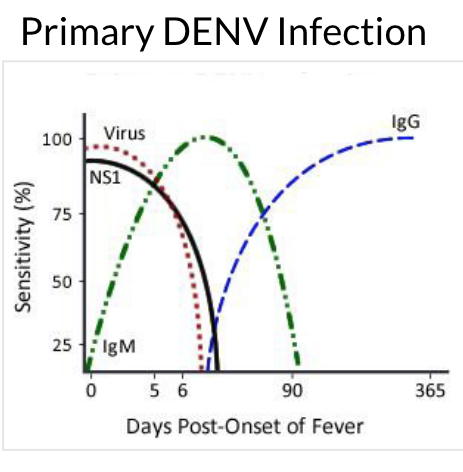
But they are effective for only a limited window of time. As our bodies clear out the acute viral infection, the level of virus in the blood drops to zero. As this chart from the CDC shows, the blood level of dengue virus becomes undetectable within a week:
From Laboratory Guidance and Diagnostic Testing
But the levels of antibody (IgM and IgG) rise and persist for much longer. Tests that detect antibody responses are known as serology tests. They use a virus or viral protein to capture and detect anti-viral antibodies from the blood.
Although the CDC chart above implies that IgG serology tests attain 100% sensitivity, this is a bit too optimistic. A fairly extensive WHO study showed that ELISA tests (which take hours and have to be performed in a lab) have sensitivities of 65–98%. Rapid tests, which can be performed in low-resource clinics near patients, have sensitivities of 20–98%.
All of the tests have poor or mediocre specificities, meaning they have false-positive rates of 2–25%. As is usual in diagnostics, the most sensitive tests are the least specific and vice-versa. Overall accuracies of the tests are no better than 85%. Previous infections with malaria or other flaviviruses (the class of virus to which Dengue belongs, along with Zika, West Nile, and Yellow Fever) are a principal cause of cross-reaction.
Why does this matter? We still don’t have a good vaccine for Dengue, and the number of virus serotypes and the incidence of infection is steadily spreading:
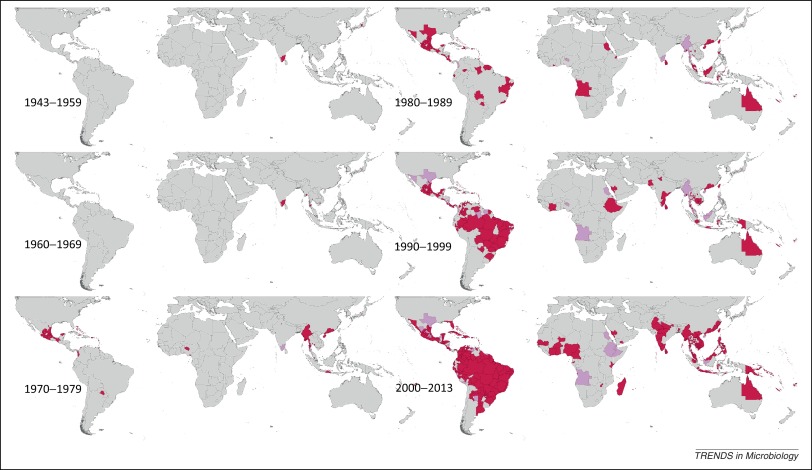 From Global spread of dengue virus types: mapping the 70 year history
From Global spread of dengue virus types: mapping the 70 year history
It appears that prior infection history affects vaccine safety and efficacy: If you haven’t had dengue infection, don’t use our vaccine, drug company warns
Vaccines are an unusual medicine in that they are given to healthy people. The level of risk that is acceptable for a vaccine is much much lower than for other medicines.
Now think about those Dengue tests. They have a 10% false-positive rate. If you try to identify people who will benefit from your vaccine – those who have already had Dengue – by testing them, you will get a lot of positive results from folks who never had it. Maybe even a majority. There’s a good chance that even with conscientious screening of vaccine candidates, the vaccine will do more harm than good.
That sucks. This is one of the reasons that vaccine development is such a difficult (and often unprofitable) business.